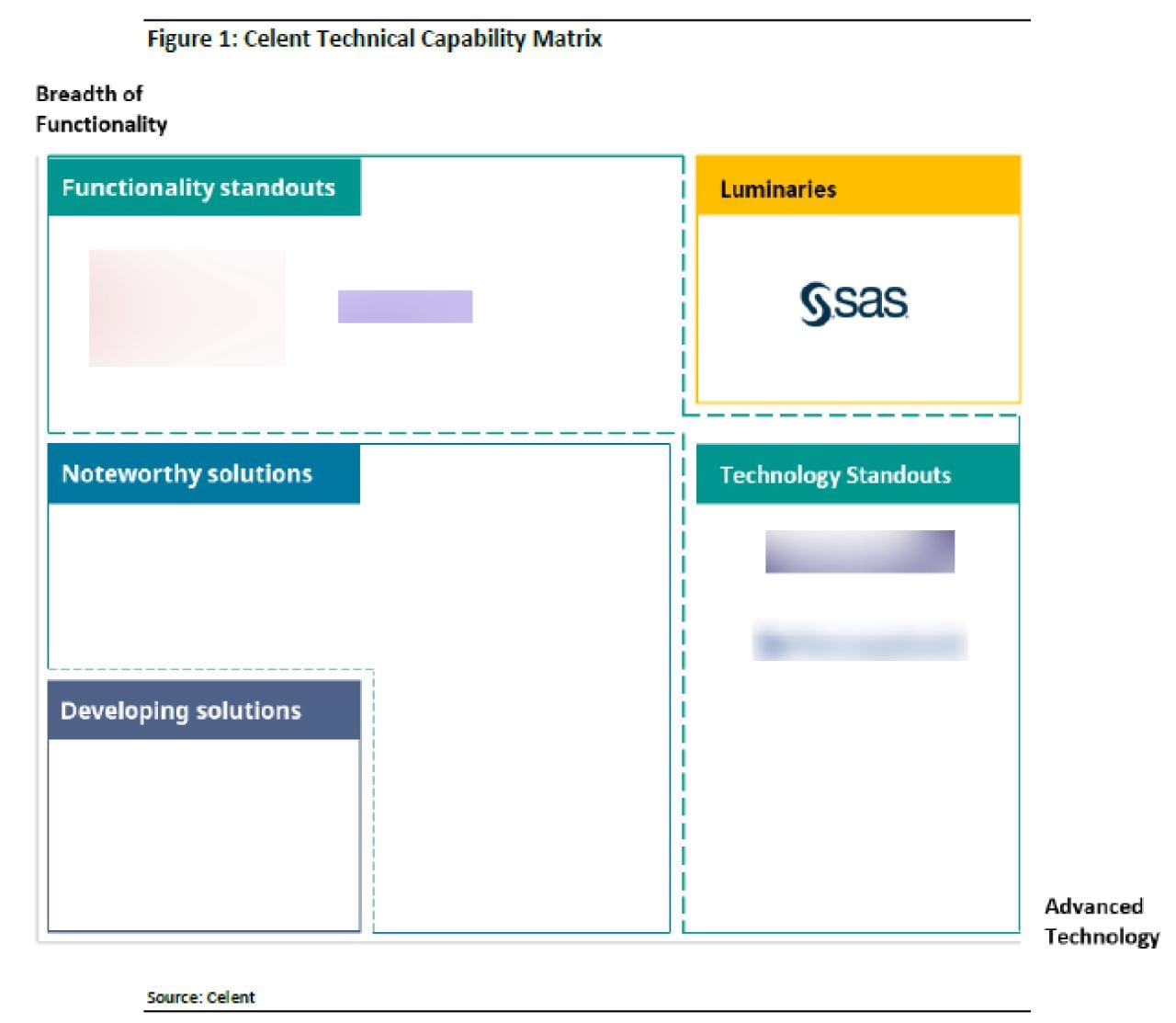
SAS IS A LUMINARY
Celent Insurance Fraud Detection Solutions: Health Insurance, 2022 Edition
Luminary: Excels in both Advanced Technology and Breadth of Functionality.
Explore More SAS Resources
To browse resources by type, select an option below.
-
- Select resource type
- Analist Raporu
- E-Kitap
- Rapor
- Rapor
- Makale
- Blog yazısı
- Kitap Alıntısı
- Kullanım Örneği
- İnfografik
- Röportaj
- Araştırma
- Seri
- Video
- Web Semineri
- MÜŞTERİ HİKAYESİ
-
Makale Analytics for prescription drug monitoring: How to better identify opioid abusePrescription drug monitoring programs (PDMPs) are a great start in combating abuse of prescription drugs, but they could be doing much more. Better data and analytics can inform better treatment protocols, provider education and policy decisions – and save lives.
-
MÜŞTERİ HİKAYESİ A risk-based approach to combat money laundering in IsraelSAS Anti-Money Laundering helps Ayalon Insurance monitor suspicious activity and meet challenging regulatory requirements.
-
Analist Raporu Celent: Insurance Fraud Detection Solutions: Health Insurance, 2022 EditionSAS was named a Luminary in Celent's Insurance Fraud Detection Solutions: Health Insurance, 2022 Edition, excelling in both Advanced Technology and Breadth of Functionality.
-
Rapor Fraudsters love digitalBy incorporating fraud analytics as a first line of defense, insurers can build in safeguards for all of their digital programs. In turn, they can spot emerging fraud rings, emerging fraud trends, and make real-time decisions on claims recovery to reduce leakage.
-
E-Kitap On the Road to Accelerating Claims AutomationMore than ever, insurance companies need to provide customers with seamless interactions that save them time, minimize hassle, and make them feel seen, understood, and cared for. Many are also exploring the use of AI for claims prevention – for example, by creating new risk mitigation services. All of this requires investment in digital technologies that work together to enable intuitive, Amazon-like customer experiences. This ebook explores how insurers can make the leap to digitally transformed, intelligent claims processes that customers love and increase operational efficiency and reduce costs.
-
Analist Raporu SAS is a Leader in The Forrester Wave™: Enterprise Fraud Management, Q2 2024
-
MÜŞTERİ HİKAYESİ Aksigorta SAS Fraud Framework çözümüne yatırım yapma kararı verdiAksigorta Fraud Projesi’nin canlıya alınmasından sonra; fraud yakalama oranı %66 arttırılmıştır.
-
Analist Raporu Chartis RiskTech Quadrant for Watchlist and Adverse Media Monitoring 2024
-
MÜŞTERİ HİKAYESİ Protecting policyholders through better fraud analysisEthniki Insurance prevents fraud, reduces costs and increases customer satisfaction with SAS Detection and Investigation for Insurance.
-
Rapor 2021 State of Insurance Fraud Technology StudyAs fraud continues to frustrate survey respondents, it's not surprising that the adoption of insurance anti-fraud technologies among respondents grew since the 2018 survey.
-
MÜŞTERİ HİKAYESİ Advanced analytics can detect and prevent insurance fraud before losses occur
-
Makale 6 ways big data analytics can improve insurance claims data processingWhy make analytics a part of your insurance claims data processing? Because adding analytics to the claims life cycle can deliver a measurable ROI.
-
MÜŞTERİ HİKAYESİ Turkish insurer achieves real-time fraud detectionAksigorta uses advanced analytics to increase fraud detection rate by 66 percent.
-
Makale Are you covering who you think you’re covering? How rigorous are you in determining membership eligibility? By some estimates, between 4 and 18 percent of all health plan benefits are paid in error due to eligibility fraud issues.
-
Rapor Effective fraud analytics: 10 steps to detect and prevent insurance fraudInsurers that follow the 10 steps outlined in this paper offer the best chance for detecting both opportunistic and organized fraud.
-
Analist Raporu Celent Insurance Fraud Detection Solutions: Property and Casualty Insurance, 2022 EditionSAS is a Luminary in Celent's Insurance Fraud Detection Solutions: Property and Casualty Insurance, 2022 Edition.
-
Makale Shut the front door on insurance application fraud!Fraudsters love the ease of plying their trade over digital channels. Smart insurance companies are using data from those channels (device fingerprint, IP address, geolocation, etc.) coupled with analytics and machine learning to detect insurance application fraud perpetrated by agents, customers and fraud rings.
-
Rapor Fighting Insurance Application Fraud Learn about the advantages of using analytics-driven methods for authenticating applicants to reveal customer gaming, agent gaming and potential future claims fraud.